The Oliphant in the room
How credible are New Zealand's guidelines on gender healthcare for young people?
What’s guiding the New Zealand approach to gender healthcare for young people?
The rates of children and young people seeking gender-affirming healthcare have grown enormously over the last decades. In considering treatment options New Zealand ministries and officials rely on the 2018 Guidelines for gender affirming healthcare for gender diverse and transgender children, young people and adults in Aotearoa.
The Guidelines are published by the University of Waikato’s Transgender Health Research Lab and written by Jeanne Oliphant, Jaime Veale, Joe Macdonald et al. The Oliphant Guidelines set the approach used by health providers across the country. A version of the guidelines has been published in the New Zealand Medical Journal. Te Whatu Ora, the Ministry of Health, The New Zealand Psychological Society, NZ Doctor and Pharmac all defer to Oliphant et al. Gender lobby and support groups including InsideOUT, Gender Minorities Aotearoa, and Te Ngākau Kahukura uphold the Guidelines. The Guidelines are also referenced in policy statements unrelated to health by, among others, the White Ribbon campaign, the Broadcasting Standards Authority and the Human Rights Commission.
But what if these enormously influential guidelines are wrong? What if there’s no good evidence that gender affirmation actually helps young people? What if, in the haste to support an unverified theory about what best works for young people, the usual medical safeguards and requirements for evidence have been disregarded? What if no one checked if the Guidelines are medically or ethically sound?
Common sense alone would cast doubt on the credibility of Oliphant et al. The name—Guidelines for gender-affirming healthcare for gender diverse and transgender children, young people and adults in Aotearoa—already assumes that gender affirmation is the only appropriate treatment or pathway. It bears no sign of the clinical scepticism or professional curiosity of good scientific thinking. The Guideline authors have already decided what should be done and only seek to explain how.
Further, the Guidelines are based on the World Professional Association of Transgender Health (WPATH) Standards of Care (SOC) The latest version, SOC 8, makes for disturbing reading. It argues that other issues presenting alongside dysphoria must not become a barrier to gender-affirming care (pp S172:S176). Depression, undiagnosed autism, a history of sexual abuse or homophobic bullying are, it would seem, no reason to stop medical interventions focused solely on gender identity. Exploring how identifying out of one’s sex might be related to or even arise directly from these issues is considered damaging. The Oliphant guidelines continue this theme and are particularly keen to ensure neurodiverse people aren’t blocked from transition.
“It is important to acknowledge that the person presenting is the expert on their own experience. Although some neurodiverse people may have difficulty in articulating their gender identity, this should not create an unnecessary barrier to access any relevant gender affirming services. Some people may express their gender identity non-verbally.” (Oliphant et al, p23)
So keen to remove obstacles to medical transition, SOC 8 removes recommendations around the lower age limit for any gender medicine or surgery (Medscape, 2022). SOC 8 also has a chapter dedicated to ‘eunuch’ as a gender identity. This chapter, in full seriousness, discusses what surgical and hormone options should be offered to those who identify as eunuch, including the removal of all genitalia and sexual functioning. In discussing the legitimacy of eunuch individuals SOC 8 references the Eunuch Archives, a long-running pornographic eunuch fetish website, in which the standard narrative of the stories is that young men are turned into eunuchs against their will (SOC 8, pS88).
Chemical or surgical castration may be experienced as a source of distress to cis men with prostate cancer, while the same treatment may be affirming and a source of comfort for eunuch individuals…Following an assessment as per the SOC-8, medical options requested by the patient can be considered and prescribed, if appropriate. These options can be tailored to the individual to create a plan that reflects their specific needs and preferences. (SOC 8, pS90)
If there’s any doubt that the NZ guidelines just missed the obvious red flags and weirdness of SOC 8, a co-author of SOC 8 is Jaime Veale. Veale is secretary of WPATH, runs the Transgender Health Research Lab which published the Guidelines, and is president of WPATH’s local little brother, the Professional Association of Transgender Health Aotearoa (PATHA).
The Cass Report
In 2020, the UK’s National Health Service (NHS) commissioned renowned paediatrician Dr Hilary Cass to run the Independent Review of gender identity services for children and young people. In March of this year, Cass published her Final Report.
The Cass Review took four years, and involved systematic reviews of evidence undertaken by the University of York (systematic reviews are the gold standard for medical evidence), other qualitative and quantitative research, focus groups and discussions with clinicians, parents and patients. Cass found there was no solid evidence that gender-affirmation was beneficial. Gender medicine, said Cass, was built on ‘shaky evidence'. There is not, she suggested, sufficient evidence to justify the use of puberty blockers. Neither is there evidence to support the often-cited claims that puberty blockers and cross-sex hormones reduce suicidality, reduce gender dysphoria or improve body image. There is only weak evidence to suggest they improve mental health.
Cass gave weight to growing concerns that there was not enough evidence to keep giving kids puberty blockers. England, Northern Ireland, Scotland, Sweden, Finland and France have all pulled back from or stopped puberty blocker prescriptions. Most UK medical institutions have endorsed Cass. When the British Medical Association last month tried to reject Cass’s findings it appeared to do so without support of its membership. To date, 1400 people have signed a letter of protest, 900 of whom are BMA members. Signatories include at least 57 professors and 22 former or current presidents of royal medical associations.
Assessment of the Oliphant guidelines
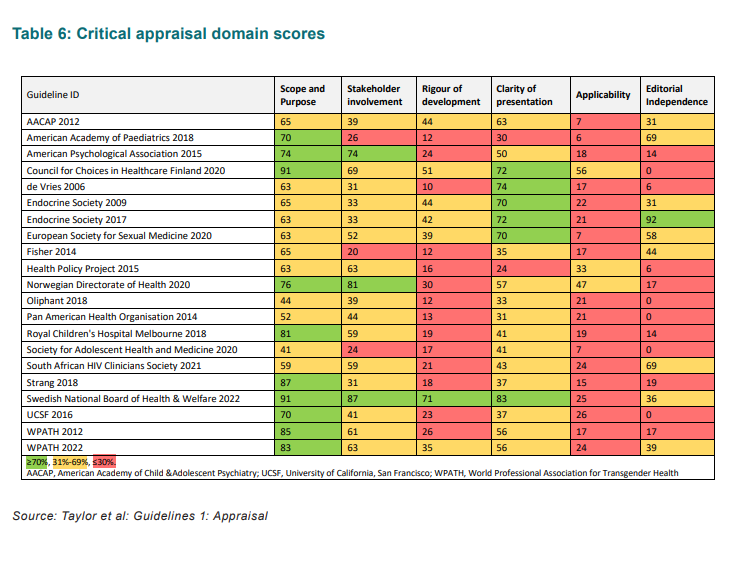
Of particular relevance to this conversation, one section of the Cass Report (pp126:132) is based on an appraisal and synthesis of 23 national or international guidelines for gender healthcare for young people. Guidelines were assessed against six domains using the AGREE II standards, the common global standard used to assess clinical guidelines.
The review of the guidelines was damning. The authors concluded that:
“Most clinical guidance for managing children/adolescents experiencing gender dysphoria/incongruence lacks an independent and evidence-based approach and information about how recommendations were developed. This should be considered when using these to inform service development and clinical practice.”
Among the guidelines assessed were New Zealand’s Oliphant Guidelines.
The WPATH SOC 7 and SOC 8 met just one of the six standards which would make them considered suitable to be used in practice. The New Zealand guidelines met none of the standards. In fact, out of the 23 guidelines assessed, Oliphant et al received the second to lowest scores. Notably, it achieved only 12% on Rigour of Development, 21% on Applicability and 0% on Editorial Independence.
The backbone of New Zealand’s approach to gender-related healthcare, that which unquestioningly promotes gender affirmation, is not fit for purpose. According to the University of York, the Oliphant Guidelines fail to meet the standard that allows them to be recommended for clinical use.
New Zealand response
PATHA and various New Zealand gender lobby groups have, like their overseas counterparts, tried to smear Hilary Cass and her report. They’ve imported, often word-for-word, critiques of the report as anti-trans, methodologically flawed, and against consensus. Like Australian counterparts, they’ve tried to argue that Cass just doesn’t apply here in NZ. It’s understandable. There are entire organisations, careers, reputations and livelihoods that rest on the presumed efficacy of gender affirmation.
Hilary Cass has gone to considerable lengths to counter inaccurate statements about her report (Cass FAQ, 2024). She’s also talked about the toxicity of the debate and is deeply angry about the misinformation that is being spread by organisations like PATHA and InsideOUT.
“If you deliberately try to undermine a report that has looked at the evidence of children’s healthcare, then that’s unforgivable. You are putting children at risk by doing that.” (Hilary Cass, 2024)
Why are New Zealand officials continuing to let discredited guidelines dictate the treatment of our children and young people? Why are they continuing to support organisations that are trying to shut down evidence?
NZ officials are certainly aware of the Cass Report. It’s not the first warning they’ve had about the lack of evidence for New Zealand’s approach. Epidemiologist and emeritus professor, Charlotte Paul, has raised questions on multiple occasions. Paul’s urgent concern is fuelled in part by our high puberty blocker prescription—some 11 times the rate of the UK. (Paul, North & South, 2024).
Cass gives us more than enough reason to rethink Transgender Health Research Lab’s privileged position in establishing and influencing clinical practice in New Zealand. It’s shoddy. Such a rethink doesn’t seem to be happening. An evidence brief on puberty blockers, first due in April of 2023, has now been postponed at least three times. It’s been reviewed by Dr Sue Bagshaw, a Christchurch doctor and outspoken advocate for puberty blockers. Te Whatu Ora has, meanwhile, commissioned none other than PATHA to update national guidelines and referral pathways for transgender healthcare. Gender-affirming interventions continue apace.
Never mind the evidence. Never mind the kids.
Key documents
Guidelines for gender affirming healthcare for gender diverse and transgender children, young people and adults in Aotearoa, Oliphant J, Veale J, Macdonald J, Carroll R, Johnson R, Harte M, Stephenson C, Bullock J. Transgender Health Research Lab, University of Waikato, 2018.
WPATH Standards of Care for the Health of Transgender and Gender Diverse People, Version 8, World Professional Association for Transgender Health, 2022.
Final Report. The Cass Review: Independent review of gender identity services for children and young people, National Health Service, April 2024.
Systematic Reviews, Gender Identity Service Series, University of York, 2024.
A terrible trap, Charlotte Paul, North & South, December 2023.